Technology Overview
ACN Healthcare’s Technology Practice focuses on identifying and delivering unique solutions for Healthcare Organizations. We provide Business Intelligence Dashboards (available on the iPad). Product Development, Support Services and Automation tools for our customers as well as our internal staff.
ACN Healthcare AR Claims Check and Eligibility Check
ACN’s AR Claims Check and Eligibility Check are productivity tools that were built to connect directly to a payer’s website to retrieve data on patient eligibility and claim status. It was designed to improve the customer satisfaction by ensuring accurate information and payment times for health care providers.
The technology can be used by organizations for individual transactions or as part of a web-based tool that provides an automated, “no touch” approach to eligibility retrieval and claims status with dramatic enhancements in staff productivity.
A single instance of our application will check a Payer Website and retrieve up to date payer/claim information into any database (mySQL, SQL2012, etc.). Depending on the number of fields, the program will check an average of 5 accounts per minute / 300 per hour / 2,400 per day.
These are AR Accounts – which no longer require a User to spend time looking up each account via the web. The results can then be imported into a billing system – and workflow will direct the claims where the need to go (i.e. Medical Record, Re-Submit, Payment Made, etc.)
New Payers can be added quickly by end-users and do not require programmer support.
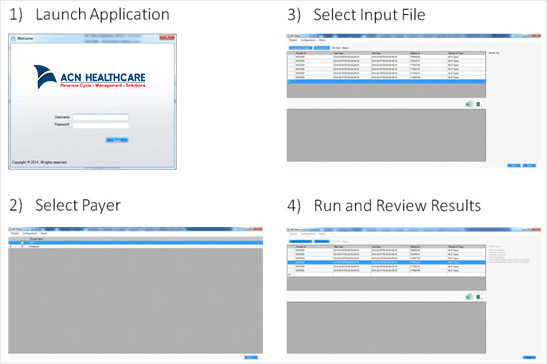
To further enhance the User experience, we kept the application workflow simple as shown below: